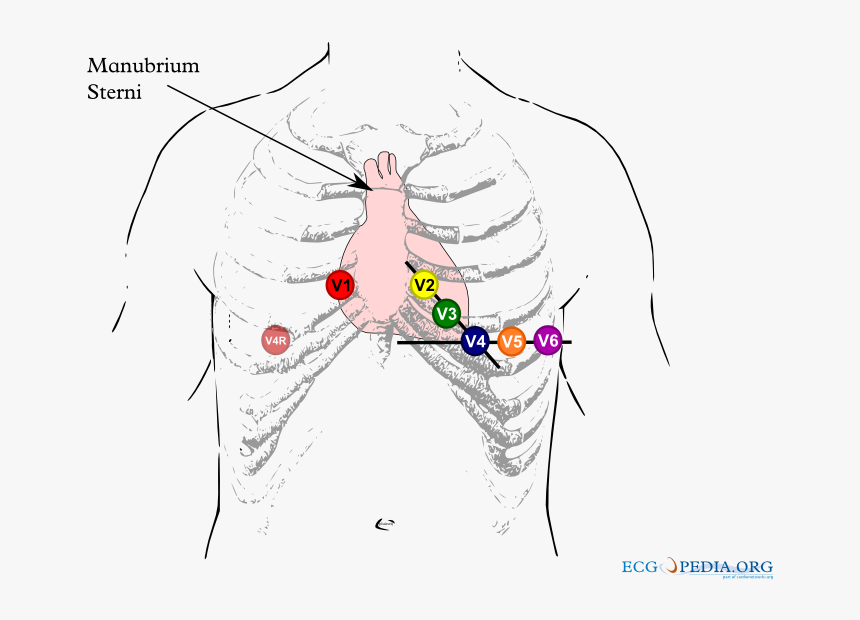
brugada ecg lead placement
80 of Brugada syndrome diagnosed only after a cardiac arrest. To assess the feasibility and reliability of using high precordial lead ECGs in conjunction with three new criteria for identifying true.
Brugada Syndrome Ecg Placement Hd Png Download Kindpng
Standard 12-lead ECG with V1V3 recorded from the fourth intercostal space and an additional.

. V1 and V2 should be placed at the 4th intercostal space. Brugada_lead_placementpng 800 600 pixels file size. This ECG was recorded.
There is rSr in both V1 and V2 with a saddleback in lead V2 and the beta angle is wide. Having just written on this topic I knew that this could be the result of lead placement that is too high. Brugada Syndrome is a rare inherited cardiac arrhythmia syndrome that is characteristed by a coved-shaped atypical right bundle branchpattern on a 12-lead ECG Type-1 Brugada pattern ECG and is associated with ventricular arrhythmias and sudden cardiac death.
The positivity was defined as inducible Type 1 Brugada pattern in atleast 2 right sided leads. The type 1 Brugada ECG pattern is characterized by a complete or incomplete right bundle-branch block pattern with a coved morphology ST-segment elevation of at least 2 mm in the right precordial leads V 1 V 3 followed by a negative T wave. The most typical and diagnostic is type 1 Brugada syndrome.
It has been recognized as a clinical entity since 1992. A programmed electrical stimulation was performed on our patient and a sustained ventricular arrhythmia. Brugada Type 2 Not Type 1 V1 and V2 may be placed in the 3 rd or even 2 nd intercostal spaces in order to elicit a type 1 Brugada pattern and is considered diagnostic.
Please see the file description page for further information. ECG recordings and even more with placement of precordial leads V1V2 and V3 in the 2 nd and 3 rd intercostal space which may bring out a typical Brugada pattern and should be routinely performed when the diagnosis is suspected but is uncertain on a standard ECG and in screening of family members of BS patients. Brugada syndrome is a rare inherited arrhythmic disorder causing an increased risk of syncope and sudden death due to ventricular fibrillation.
The Brugada syndrome may present with three different ECG patterns referred to as type 1 type 2 and type 2 Brugada syndrome ECG. Brugada Syndrome is reported to be responsible for 4 of all sudden deaths and 20. The incidence of this disease is on the order of 5 per 10000 inhabitants and it.
Brugada Syndrome is an ECG abnormality with a high incidence of sudden death in patients with structurally normal hearts. Demonstration and unmasking of the type 1 ECG pattern at the higher lead positions also have diagnostic value for Brugada syndrome similar to its. The diagnosis of the characteristic type-1 or coved type Brugada ECG figure 1 is made from the right precordial ECG leads see also Wilde 2002.
Resting 12-lead ECG with standard precordial leads and ECG with precordial leads placed 1 Intercostal space above were performed after flecainide administration every 5 min for first 30 min and every 30 min thereafter until ECG became normal or upto 6 h. By contrast a type 2 Brugada pattern may often be found with these high leads are applied to healthy people especially in fit young males. Proven VF or VT.
12 To ensure consistent lead placement we incorporated a high precordial lead V1 and V2 at the 2nd intercostal space ECG into our. First described in 1992 by the Brugada brothers the disease has since had an exponential rise in the numbers of cases reported. When gaining a 12-Lead ECG a configuration wherein the placements of V1 and V2 are positioned more cranially V1 ICS12 V2 ICS12 should be recorded as these leads can often give a clearer view of abnormal morphologies.
The type 2 ST-segment elevation has a saddleback appearance with a high takeoff ST-segment elevation. B Spontaneous type 1 Brugada ECG pattern in a 53-year-old man with aborted cardiac arrest implanted ICD and subsequently multiple appropriate shocks of the device. Brugada syndrome requires BOTH 1 Brugada ECG pattern and 2 clinical criteria.
Aims The authors sought to assess the value of the high right precordial leads RPL to detect the Type I Brugada ECG pattern in patients suspected of carrying Brugada syndrome BrS. Imagepng This file is from a shared repository and may be used by other projects. The use of precordial leads in the 2nd or 3rd intercostal space has been described in patients with suspected and known Brugada syndrome5 11.
Here is an example of type I Brugada pattern during fever that disappeared after antipyresis. Consider as cause of syncope in patients with family history of sudden death. The Brugada syndrome is an autosomic dominant genetic disease.
It features large coved ST-segment elevations and T-wave inversions in leads V1V3. It meets or at least nearly meets criteria for type 2 Brugada. Sensitivity of the ECG can be increased with alternative placement of ECG leads to the intercostal space above V1 and V2 figure 2.
A higher right precordial lead placement than the conventional position at V1V3 can also be used to unmask the Brugada-type ECG in subjects without typical ECG changes or unequivocal signs. And the caveats of improper lead positioning were recently reviewed. Brugada syndrome is a condition which can lead to polymorphic ventricular tachycardia ventricular fibrillation and sudden death.
A Fractionated QRS complex in a 25-year-old asymptomatic male patient with BrS ajmaline-induced type 1 Brugada ECG pattern. Careful placement of leads is essential to avoid false positive findings. It is characterized by ST segment elevation in the right precordial leads V1-V2 and a high incidence of sudden death in patients with structurally normal heart due to ventricular arrhythmias 2.
An rSr pattern in leads V1-V2 can be observed when ECG leads are placed in the 2nd intercostal space. 84 KB MIME type. The mean age of sudden death is 41 with the age at diagnosis ranging from 2 days to 84 years.
Lead V1 from the 4th 3rd and 2nd ic. Placement of the right precordial leads in a superior position up to the second intercostal space above normal can increase the sensitivity of the ECG for detecting the Brugada phenotype both in the presence or absence of a drug challenge. Recently three criteria analyzing the ST segment and r width to identify true Brugada pattern ECGs have been described.
Diagnosis can only be considered appropriate with a positive ECG as well as at least one of the following. A typical baseline Fig A and positive ECG Fig B are shown. Conclusion In our athletes without preexisting incomplete RBBB a Brugada-like pattern was easily obtained and highly prevalent with high placement of anterior precordial leads.
Methods Ajmaline testing using 15-lead ECGs was performed in 183 patients suspected of carrying BrS. Identifying it before death is important. Brugada Syndrome is an abnormal ECG Right Bundle Branch Block Pattern with coved ST elevation over the right precordial leads of V1-V3 which leads to ventricular fibrillation VF and sudden cardiac death SCD in patients with structurally normal hearts.